NIAID Launches First Clinical Trial to Test Antibody–Drug Combination for Long-Acting HIV Treatment
Cross-posted from NIAID Newsroom
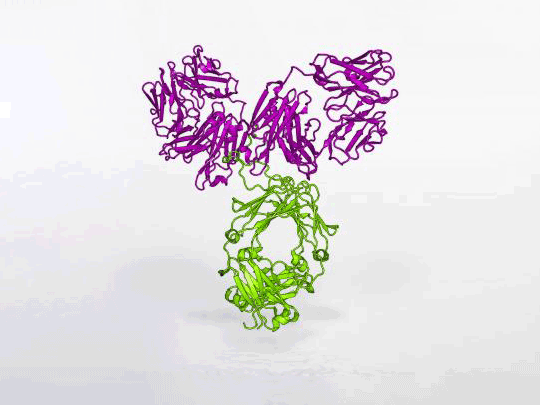
Credit: NIAID
The first clinical trial to test the combination of a long-acting anti-HIV drug plus a powerful HIV antibody as a long-acting treatment for people living with HIV has begun. Investigators are studying whether long-acting cabotegravir and an antibody called VRC07-523LS are safe and tolerable and prevent HIV from rebounding to detectable levels in people who previously kept the virus suppressed with daily antiretroviral therapy. NIAID is sponsoring and funding the Phase 2 trial, called A5357, which is being conducted by the NIAID-funded AIDS Clinical Trials GroupExit Disclaimer (ACTG).
Current treatment for HIV involves taking two or more antiretroviral drugs in tablet form daily, often as a single pill. Sticking to a daily drug regimen can be difficult for some people, however, so scientists are researching new HIV treatment regimens that involve a dose of medication just once a month or even less frequently. Already, two Phase 3 clinical trials have demonstrated that a monthly injection of long-acting formulations of the antiretroviral drugs cabotegravir and rilpivirine effectively treats HIVExit Disclaimer in adults.
While some scientists are developing long-acting formulations of antiretroviral drugs, other researchers are exploring the potential of powerful anti-HIV antibodies as a form of long-acting HIV treatment. These antibodies, which some people with HIV naturally produce a few months or years after acquiring the virus, are described as “broadly neutralizing” because they can stop a wide variety of HIV strains from infecting immune cells in the laboratory. Investigators have begun clinical trials of pairs of these broadly neutralizing antibodies, or bNAbs, for both long-acting HIV treatment and HIV prevention.
A5357 differs from these other studies because it is pairing a long-acting antiretroviral drug with a long-acting bNAb, each of which thwarts the virus in a very different way. The antiretroviral drug, cabotegravir, interrupts HIV replication within a cell by preventing viral DNA from integrating into the cell’s DNA. The bNAb, VRC07-523LS, prevents HIV from entering a cell in the first place by binding directly to the virus at its cell-docking site. Although HIV is known for rapidly mutating to escape obstacles to replication, it is unlikely to develop mutations that enable it to escape both blocking strategies.
Scientists at the NIAID Vaccine Research Center engineered VRC07-523LS based on a naturally occurring bNAb that they identified and isolated in 2010. The engineered antibody neutralizes 96% of HIV strains on a globally representative panel, binds very tightly to the virus, lasts for an extended period in blood plasma, and appears in higher concentrations in mucosal tissue.
The leaders of the A5357 trial acknowledge that the combination of VRC07-523LS and long-acting cabotegravir would not be ideal in real-world clinical practice because each agent has a different route of administration and dosing schedule—cabotegravir by injection every 4 weeks and VRC07-523LS by infusion every 8 weeks. However, scientists and volunteers are undertaking the A5357 trial to gain valuable insight into whether the concept of combining a bNAb with an antiretroviral drug is successful as a long-acting HIV treatment strategy. Investigators are hopeful that better bNAb–antiretroviral drug combinations will become available for clinical testing in the future.
The ideal bNAb–antiretroviral drug combination would be self-administered as a single shot under the skin, the way people with diabetes give themselves insulin, every 8 weeks or more. Also, developing resistance to the ideal long-acting combination would be so difficult that a person could keep HIV suppressed even if they missed a dose by several weeks.
The A5357 trial will take place at 18 sites in the United States and Puerto Rico. The study team will enroll 74 people ages 18 years or older who are living with HIV and have been taking daily antiretroviral therapy that has kept the virus suppressed for two years or more. Only people whose HIV is susceptible to the VRC07-523LS antibody, based on a blood test, will be eligible to enroll.
Upon entering the study, participants will discontinue part of their current antiretroviral regimen and start taking daily oral cabotegravir. Those who tolerate this drug and still have a suppressed level of HIV at their fourth or fifth week in the trial will discontinue daily oral antiretrovirals and start receiving the experimental treatment regimen. This will consist of an injection of long-acting cabotegravir once every 4 weeks and an intravenous infusion of VRC07-523LS once every 8 weeks. Participants will remain on this experimental treatment regimen for 44 weeks. The study team will test the level of HIV in participants’ blood (their viral load) every 2 to 4 weeks. At the end of this 44-week period, or sooner if the virus rebounds to a detectable level, participants will resume taking daily oral antiretroviral therapy and will have their viral load monitored for 48 more weeks. Results are expected in 2022.
ACTG is conducting A5357 under the leadership of Babafemi Taiwo, M.B.B.S., and Pablo Tebas, M.D. Dr. Taiwo is chief of infectious diseases and the Gene Stollerman Professor of Medicine in the Feinberg School of Medicine at Northwestern University. Dr. Tebas is a professor of medicine in the Hospital of the University of Pennsylvania. ViiV Healthcare is donating oral and injectable cabotegravir for the trial. Monogram Biosciences is performing the testing to determine if the HIV in potential participants’ blood cells can be killed by VRC07-523LS.
More information about the A5357 trial is available at ClinicalTrials.gov under study identifier NCT03739996.